Experiences of bihormonal fully closed-loop system in T1D
Giesje Nefs, Theodorus J P Jansen, Michel Klaassen, Lyan B Vlaskamp, Mattijs Out, Gozewijn D Laverman, Bas J J W Schouwenberg, Martin N Gerding, Alexandra H Mulder, Mechteld A R Vermeulen, Jeroen P H van Wijk, Frank J Snoek, Helga Blauw, J Hans DeVries, Arianne C van Bon
User Experiences of a Bihormonal Fully Closed-Loop System Among Adults with Type 1 Diabetes in a Real-World Setting: A Qualitative Analysis. Diabetes Technol Ther. 2025 Oct 7.
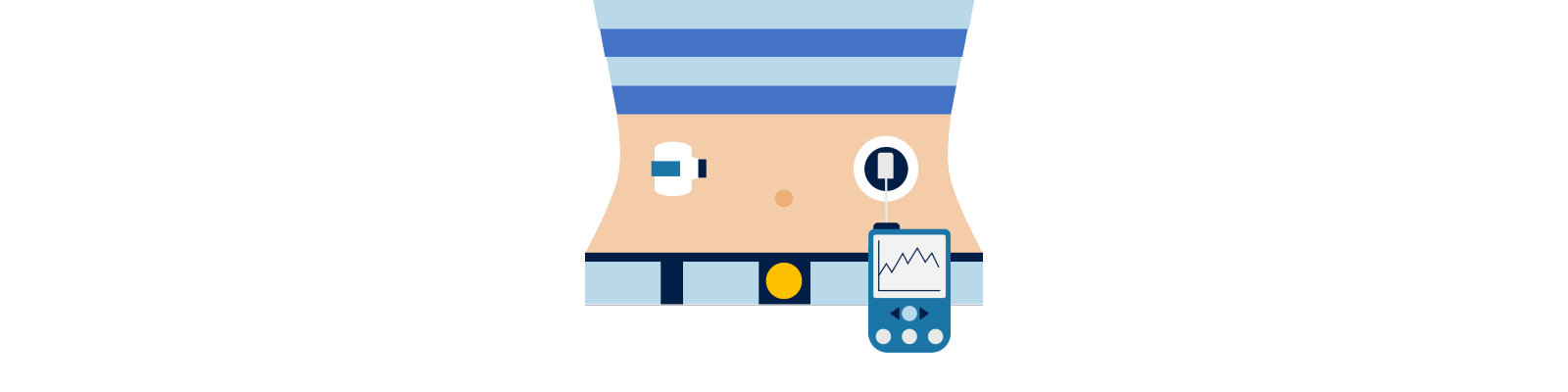
Automated insulin delivery systems are increasingly recommended for adults with type 1 diabetes because they improve glycaemic outcomes and reduce the burden of day-to-day management. Hybrid closed-loop systems still require frequent user input, especially around meals and exercise. Fully closed-loop (FCL) systems aim to eliminate these tasks by automating insulin and glucagon delivery based on sensor data.
A recent 12-month real-world trial (FREE 1) of a bihormonal FCL system (Inreda AP®) showed substantial improvement in time-in-range and reduced diabetes distress, but also a 13% discontinuation rate, suggesting unmet user needs. To inform future implementation, this qualitative study explored how adults experienced living with the system, why they continued or discontinued, and how they balanced advantages and burdens in daily life.
Twelve adults who participated in the FREE 1 trial completed semi-structured interviews after one year of FCL use. Eight were ongoing users; four had discontinued during the trial. Participants were purposefully selected to represent different patterns of change in glycaemic and patient-reported outcomes. Interviews explored motives for starting FCL, perceived impact on life, the process of adjusting to the system, and the benefit-burden trade-off. Data were analysed thematically.
Key findings:
- People decided to start FCL hoping for improved health, reduced diabetes burden, greater freedom, and a more “normal” life.
- For most ongoing users, benefits such as improved glycaemic control and feeling less like an ill person outweighed the system’s demands.
- The system required significant ongoing effort, with a difficult start-up period described as not “plug-and-play.”
- Burdens included multiple components, frequent alarms, glucagon replacement, wearability issues, and nausea for some users.
- People who continued developed coping strategies and found an acceptable “working relationship” with the device.
- People who discontinued typically experienced early and accumulating negative experiences, leading to a tipping point.
- Expectations shaped satisfaction; overly positive external messaging contributed to frustration when real-world experiences did not match.
The findings highlight the need for realistic expectation setting, flexible and ongoing support, and design improvements that reduce alarm load, wearability challenges, and glucagon-related burdens. Clinicians and manufacturers should recognize that successful adoption requires psychological adaptation as well as technical training.
Concluding, the authors state
"FCL users experience improvements mostly in glycemic and often also person-reported outcomes, with continuation of use depending on reconcilability of technology hassles." -
Please click here for the Pubmed link.