Skin Complications from Diabetes Devices in Children
Berg AK, Passanisi S, von dem Berge T, Chobot A, Elbarbary NS, Pelicand J, Giraudo FS, Mentink R, Levy-Khademi F, Creo AL, Heidemann MS, Piona C, Arslan E, Gunes Kaya D, Sas TCJ, Krogvold L, Tumini S, Berget C, Dos Santos TJ, Karges B, Zorron M, Svensson J; ISPAD Jenious Group.
SKIN-PEDIC: A Worldwide Assessment of Skin Problems in Children and Adolescents Using Diabetes Devices. Horm Res Paediatr. 2025 Mar 24:1-14.
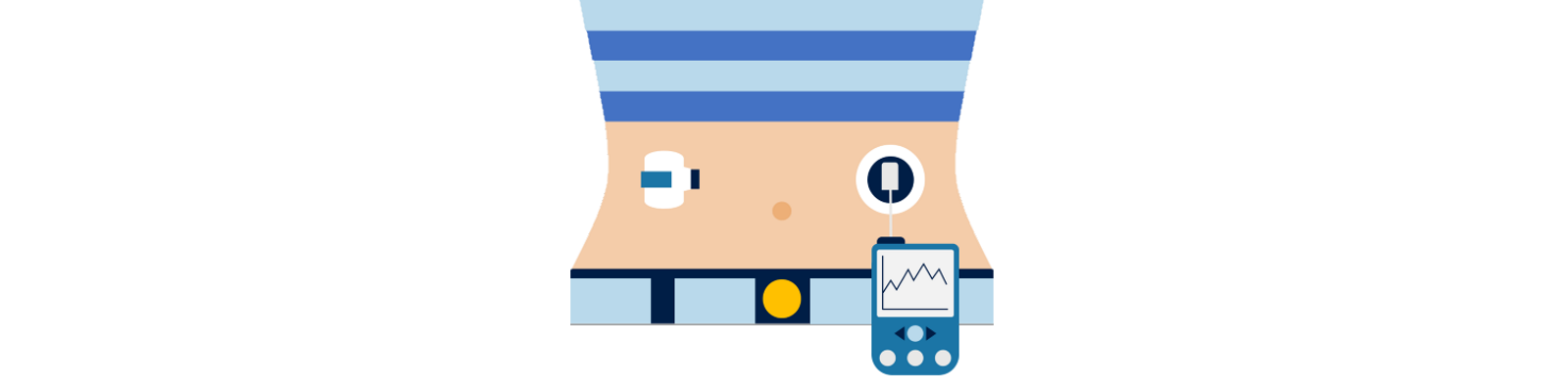
Diabetes technologies, including insulin pumps, continuous glucose monitoring sensors, and closed-loop systems, have become central to pediatric diabetes care because they improve glycaemic control, reduce acute complications, and support children’s autonomy. These benefits have led international guidelines, such as ISPAD, to recommend early adoption of diabetes technology in youth with type 1 diabetes.
However, device adhesives and insertion systems can cause a wide range of skin complications, including eczema, scarring, infection, lipodystrophy, and local irritation. These complications can lead to discomfort, reduced adherence, emotional distress, and even discontinuation of technology. Previous research on device-related skin problems has largely consisted of small, single-center studies that rely on self-report, often with limited dermatological assessment and high sampling bias. Moreover, little is known about long-term consequences in children who may use adhesive devices continuously for decades following diagnosis.
To address this evidence gap, the SKIN-PEDIC study conducted a multicenter, global assessment of skin complications using standardized, clinician-based evaluation during routine visits, aiming to quantify prevalence, identify risk factors, and inform clinical practice. The study included 1,719 children and adolescents from 22 pediatric diabetes centers worldwide over a 4-week period. Skin at pump and sensor sites was assessed by health-care professionals during routine visits, and clinical, dermatological, and device-related characteristics were recorded. The study used regression models to examine associations between risk factors and skin problems.
 KEY FINDINGS
KEY FINDINGS
- Skin problems were common, affecting roughly half of pump users and one-third of sensor users.
- Scarring and lipohypertrophy were more prevalent at pump sites than sensor sites, suggesting a greater burden with infusion-set use.
- Eczema was observed at both pump and sensor sites, indicating frequent inflammatory reactions to adhesives.
- Infections were uncommon, likely reflecting improvements in device design and user education.
- Dermatological conditions such as xerosis cutis and keratosis pilaris increased the risk of skin complications by several fold.
- Longer duration of device use was associated with more scarring, suggesting cumulative tissue damage over time.
- Preventive measures were widely used, but their effectiveness could not be determined due to the likelihood of reverse causation.
- Marked differences between centers highlighted the influence of environmental, cultural, and clinical practice factors.
The high prevalence of device-related skin problems demonstrates that dermatological complications are a significant and under-recognized barrier to sustained use of diabetes technology in children. Particular concern arises for children with atopic skin, those diagnosed at a young age, and individuals who will rely on these devices long-term. The findings support the need for improved prevention, personalized care, and device innovation that prioritizes skin compatibility alongside glycaemic performance.
CONCLUDING THE AUTHORS STATE
"This is the first global multicenter study investigating skin problems in youths using diabetes devices, emphasized the clinical relevance of skin problems as a potential major barrier toward the effective use of diabetes technology." -
Please click here to go to PubMed.