Persisting proinsulin production in T1D
Douwe Frank de Wit, Coco Marjolein Fuhri Snethlage, Rana Minab, Elena Rampanelli, Pleun de Groen, Manon Balvers, Timothy J. McDonald, Richard A. Oram, Bart O. Roep, Daniel H. van Raalte, Cameron B. Verchere, Max Nieuwdorp, Nordin M. J. Hanssen
Persisting plasma proinsulin levels in a cohort of 482 individuals with long-standing type 1 diabetes mellitus. Diabetes Obes Metab . 2025 Oct;27(10):5566-5575.
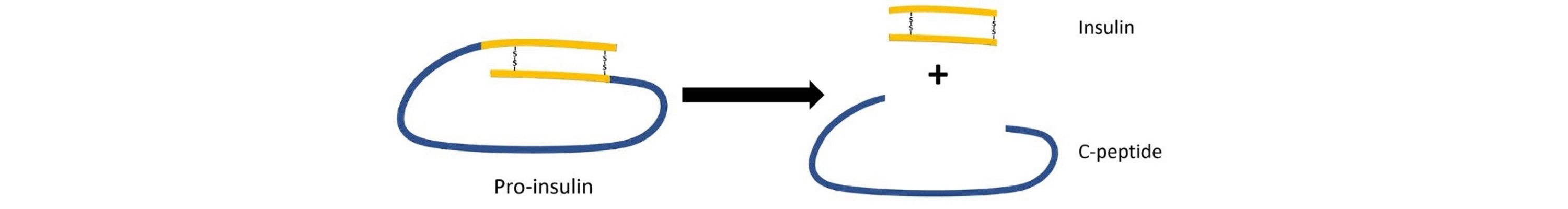
Residual beta-cell function is increasingly recognised as clinically meaningful in type 1 diabetes, as it is associated with better glycaemic control, reduced hypoglycaemia, and fewer long-term complications. Traditionally, this residual function has been assessed using C-peptide, a marker of insulin secretion. However, C-peptide primarily reflects functional insulin release and may decline due to beta-cell dysfunction rather than complete beta-cell loss.
Proinsulin, the insulin precursor molecule, may provide complementary information. Elevated proinsulin levels and a high proinsulin-to-C-peptide ratio are considered markers of beta-cell stress and impaired proinsulin processing. While proinsulin has been studied in early and preclinical type 1 diabetes, its presence and trajectory in long-standing type 1 diabetes remain poorly characterised.
This study aimed to determine whether proinsulin persists years after diagnosis, how it relates to diabetes duration compared with C-peptide, and whether immunological or genetic factors influence its decline.
The authors performed a cross-sectional analysis of 482 adults with type 1 diabetes from the GUTDM1 cohort, spanning a wide range of diabetes duration. Fasting plasma proinsulin and C-peptide were measured alongside urinary C-peptide, autoantibodies (anti-GAD and anti-IA2), and HLA genotypes. Associations with diabetes duration, beta-cell function, autoimmunity, and genetic risk were analysed using regression and spline models.
Key findings:
- Plasma proinsulin levels showed a biphasic decline, with an initial decrease over approximately 15 years after diagnosis followed by long-term stabilisation.
- C-peptide declined more rapidly, with an inflection point around 8 years after diagnosis, indicating a different temporal pattern than proinsulin.
- Proinsulin remained detectable in 69% of participants, including 59% of individuals with undetectable fasting C-peptide.
- The proinsulin-to-C-peptide ratio increased during the first 10–20 years after diagnosis, consistent with increasing beta-cell stress.
- Proinsulin and the proinsulin-to-C-peptide ratio were not associated with markers of insulin resistance such as BMI, triglycerides, or insulin dose.
- Higher proinsulin levels correlated with higher anti-GAD antibody levels, but not with anti-IA2 antibodies.
- A high-risk HLA genotype (particularly DR3/3) was associated with complete loss of both C-peptide and proinsulin.
The findings demonstrate that beta-cell activity persists in many individuals with long-standing type 1 diabetes, even when classical markers of insulin secretion are absent. Proinsulin appears to reflect the presence of stressed but viable beta cells, providing information that is distinct from C-peptide.
This has important implications for disease-modifying therapies that aim to preserve or restore beta-cell mass rather than insulin secretion alone. Proinsulin may serve as a complementary biomarker to identify individuals who still harbour salvageable beta cells and who might benefit from immune-modulating or beta-cell–protective interventions.
Concluding, the authors state
"In type 1 diabetes mellitus, proinsulin levels remain detectable long after diagnosis, also in the absence of C-peptide, implying the presence of stressed, yet alive β-cells" -
Please click here for the full-text version of the paper.